
Demand is soaring, budgets are at breaking point and the workforce is under ever-increasing pressure. It’s clear our health and care system is unsustainable and yet we’re failing to fully exploit one of our biggest assets – digital technology.
To use a sporting analogy, it’s like leaving out your best player or, at best, playing them out of position.
Drawing on Channel 3’s experience of working with health and social care systems across the country, we can see a consistently unhelpful trend emerging in how digital is being deployed.
While it’s increasingly recognised as a key enabler in unlocking a preventative and sustainable model of health and social care, it’s simply not having the impact it should have.
There are multiple reasons. Too often digital interventions are small-scale and targeted rather than being embedded in a strategic transformation journey. They’re frequently delivered in silos and resourced through central government funding pots overly focused on the technology rather than what it achieves in the long term.
To stimulate constructive debate and facilitate action on the ground, Channel 3 has created a digital blueprint for health and care that positions transformation, rather than digital, centre stage.
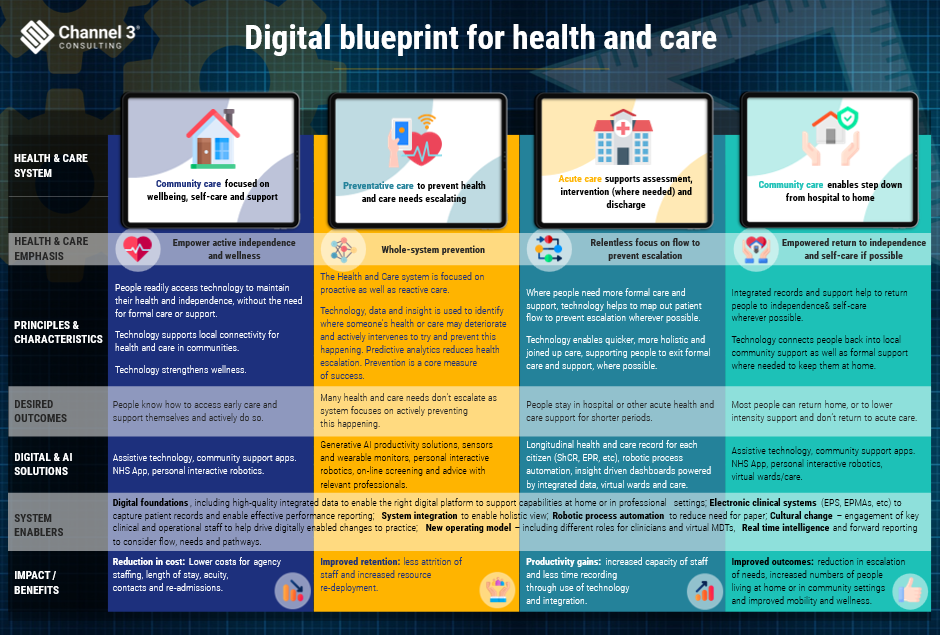
In a nutshell, it’s about framing discussions around a person’s journey through health and care, being clearer about the outcomes we’re trying to achieve, and putting digital at the heart of a strategic transformation journey. Ultimately, it is about transforming models of care through digital.
It’s a work in progress that will evolve over time, informed by discussions such as the one Channel 3 convened at this year’s ADASS Spring Seminar, bringing together a range of adult social care leaders – including DASSs and assistant directors – along with industry representatives and, crucially, insight from a person with lived experience.
‘Explosion of potential’
Speaking at a Channel 3-hosted event, Government advisor and former ADASS president, Sir David Pearson, set out three areas of an “investible proposition” for the next government and local authorities: digital, workforce and prevention. But he believes vital elements are not joined up and that’s why “we are not taking advantage of being in the third decade of the 21st century with all the opportunities that it affords”.
They include sharing information and records across health, social care, and housing sectors and using data to identify and act upon key areas of need. Real-time evaluation is required to understand what works.
“I think the opportunity is to do some of these things in bite-sized chunks, which a lot of local authorities and providers are doing. But the real nirvana is joining it all up and utilising the sort of explosion of potential that arises from having all those things pulled together in the local, digital strategy, that benefits the outcomes of the people who use the service and the effectiveness and efficiency of the system.”
Unsurprisingly, the current financial situation facing local government loomed large during the discussion.
Caroline Baria, DASS at Leeds City Council, described the “vicious cycle” of wanting to embrace technology but being constantly constrained by budgetary pressures.
“We keep finding ourselves going around this loop of, we know we’ve got to do something, we know we can’t do it ourselves, but there’s no money,” she explained, adding, “we’ve got to a find a way out of this.”
Those sentiments were echoed by Bill Shields, Deputy Chief Executive at Devon Integrated Care Board, who believes financial pressures have the potential to “foster bad behaviour between local government and the health sector”.
“We are in danger of shunting costs from one sector to the other rather than looking at joint solutions. So I’m really keen and enthusiastic about the work that’s being done by Channel 3 and with their support in Devon.
“I’m pleased to say that we are moving forward in a good way where we’re starting to understand the financial pressures – and the transformation that has to occur so that we can get to a much better place, which is going to be sustainable not only this year and next year but for the next 10 years.”
A new industrial revolution
Bill highlighted the potential impact of digital technology on health and social care in terms of improved services and outcomes and was one of two participants who likened it to the industrial revolution.
“We have not got enough money and we’re never going to have enough money so we’ve really got to start to think about how we do things in a very different way… The industrial revolution led to fewer people being employed and I think we’re looking at the same thing in terms of the digital revolution that we’re on the precipice of. Through AI we can employ fewer people and save a lot of money as a consequence.”
In Channel 3’s view, if AI and digital can help reduce the need for traditional social care roles and activities, that would free up much-needed workforce capacity to focus on services that need dedicated human attention.
Like the industrial revolution, we stand at a “change point”, according to Martin Samuels, DASS at Lincolnshire County Council, in that the current model “is no longer relevant and appropriate for the world that we’re operating in”.
But public service leaders “don’t really understand what we could be doing differently” in the same way that industrial leaders couldn’t have understood the ramifications of introducing electricity more than a century ago.
“I think one of the reasons we stumble with this is that we have that broad concept of digital, of new technology, and it’s terrifying because it’s too big and it’s too vague.
“Some things that Channel 3 has been doing are useful in starting to help people to get under the skin of what this actually means and make it both comprehensible and breaking it into smaller chunks that people can deal with.”
He believes the current situation has led to concern and uncertainty within the workforce, an issue reiterated by Carolyn Nice, DASS at Stockton-on-Tees Borough Council, who described a fear factor.
“I think there’s a lot of fear out there. I don’t think that social workers’ natural inclination is to run off and be digitalised. I think there is quite a lot of risk aversion and the fact that IT infrastructure in a lot of the councils is old and under-invested means there are times when you say, ‘Could I do this?’
“But the appetite is absolutely there. Everybody keeps saying ‘What about digital?’ We want to do something, but we don’t know what we don’t know and I think that’s the problem. We need to get our staff in the same place in terms of using technology because the public is already there.”
Best intentions
At the other end of the scale is the danger of rushing into investment without being clear on your objectives, as Nick Presmeg, DASS at Essex County Council, highlighted.
“The risk we’ve got is in 10 years we will have swamped ourselves with tech that isn’t interoperable because it was pursued through lots of disconnected investment propositions. I’ve seen it happen before.
“So the first thing for me is about intentionality. Actually deciding what you’re going to do, how you’ve got to do it, understanding how the process of adoption works and ensuring you have the organisational capability… otherwise, we’re going to end up with lots of little things that do little things.”
“I’m really optimistic about this but only if we approach it in a thoughtful, planned and intentional way. Otherwise, I can see us spending millions, billions even, and ending up with a plethora of solutions that don’t fit together.”
It all comes back to that issue of intentionality, as Bill Shields has discovered in Devon.
“Virtual wards are a bit of a bugbear of mine because the work that Channel 3 has done in Devon showed that even in the health sector and within the integrated care board, we had about four different ways of doing virtual wards.
“What are you measuring? Is it avoiding admission, facilitating discharge, both, or neither? When you are embarking on something like this it’s really important that you’re clear about the outcome.
“What I’ve seen in Devon and elsewhere is far too often we embark on something, whether it’s around digital or around AI, because it’s a nice shiny thing that will solve all the problems. But we haven’t actually diagnosed what the problem is in the first place so we’ve no idea what the solution is that we’re looking for.”
Torbay Council’s Divisional Director for Adult Social Care, Lee Baxter, cited the importance of “system stability” and consistent leadership to ensure momentum isn’t lost in the drive to utilise technology.
“There needs to be a continuation of development, otherwise it will be start-stop or we’ll de-prioritise it to do something else. We’ve seen it in trying to have joint records and shared data when it never quite follows through. So there’s a strategic tension issue there.
“There’s also the staffing culture. How do we take everybody on a journey and one they can believe in because they’re going to have to change the culture of the health and social care system? That’s quite an ask. In our transformation work, how do we help that culture change?”
Maximising the potential of AI
The advent of artificial intelligence (AI) – in particular, generative AI (Gen AI) – has generated a good deal of excitement about the possibilities it holds for health and social care. But its effectiveness relies on the quality of data it feeds off, as Helena Zaum, from software solutions provider Sentinel Partners, explained.
“I don’t think the optimism around AI is misplaced, but I think it’s fair to say there’s quite a lot of work to do to realise the potential. Gen AI is a step forward and could be really useful in terms of capacity and it is already being used by some local authorities to support demand management at the front door.
“It’s very important that we consider carefully what it can do is not necessarily always the same as what it should do. But Gen AI, like all other kinds of AI, relies on data and if your data is bad, your AI will be worse. The reality of bad data is that it very often has nothing to do with systems and everything to do with people. When we think about embracing this technology we must explain to staff that as data and AI become more important, the quality of the information they enter also becomes more important. We need good data that’s been gathered with consent and that is integrated, not in multiple places.”
Backed with good data, says Helena, AI can help to deliver much more tailored services for the individual and enable those in health and social care to, for example, get a single view of hospital discharge to create more personalised experiences and enable an even stronger focus on prevention at the front door.
Utilising AI and other forms of digital technology is effectively presenting practitioners with “a very good blank sheet of paper”, but expectations have to be managed because it will take time to implement the collective, integrated approach needed, according to Deborah Gidman, Head of Strategic Delivery for Adult Social Care at Torbay and South Devon NHS Foundation Trust.
“We can’t just land in AI and we can’t just land in digital – it’s not going to happen like that and it will take time. We need to harness the power we have collectively, but in the meantime, as we go through our transformation we need to think about what we do with prevention and how we manage expectations.”
Back to the topic of data, several participants highlighted the importance of not losing sight of who ultimately “owns” that information.
Tandra Forster, Director of Integrated Adult Social Care at Devon County Council, shared her first-hand experience of the health and care system when her mother fell ill:
“Mum’s fine now, but at the time it looked really drastic and we had to go to hospital in London. I was frustrated and my parents were shocked that they weren’t able to share information between two hospital sites. It just leaves you in limbo.
“When it comes to the shared care record, we just need to do it. I think part of the barrier is about us owning information and the fear of sharing it. What we’re forgetting is what that does to the person involved. So for me, it’s not just about what’s happening in Devon but what we do as a country. We could become ill somewhere else, so how do they get your records?”
Carolyn Nice echoed that feeling of frustration: “The information isn’t ours, it belongs to the person themselves. People are always gobsmacked when we say we can’t see your information from the hospital or the GP or vice versa because it doesn’t work like that.”
The human factor
The lack of joining up across the system, alluded to by Sir David Pearson at the beginning of our discussion, disempowers individuals and creates a blockage for staff.
Ultimately, it comes down to the health and social care workforce, not the technology, according to Martin Samuels.
“We need to think about reframing the role of people because, yes, we need to have technology, but ultimately this is about changing the way that people think and feel at work and it’s there for people to change using technology, rather than digital is going to save the world.”
It’s also imperative that we move beyond viewing technology as a way to mitigate crisis, according to Rich Amos. He is a member of the National Coproduction Advisory Group and West Midlands ADASS Coproduction Advisory Network and is someone with lived experience of drawing on support from three different local authorities.
“Rather than technology enabled care we need to think of how tech can empower people in a way to facilitate technology enabled lives. How does tech become an everyday feature of our daily lives to elevate possibilities? We’ve all probably got an Alexa in our home and it’s reimagined how tech can be used that is affordable, multi-functional and a mainstay.”
But the human factor is all-important and should not be neglected in our efforts to embrace technology, he says.
“We need to invest in digital because it’s the right thing to do instead of ‘because we have to’. Channel 3’s blueprint references the need for a holistic transformation approach where digital isn’t treated in isolation from the human workforce. Whilst there are clear ways in which digital can work towards enhancing productivity, we need to remember social care is built around the relationships of people to people. It’s about the nuances that enable the connections between one another and the trust that is gained which is all transformative in its own right. I wouldn’t be who I am without human support.”
Conclusion
Our ADASS Spring Seminar breakfast meeting highlighted the critical role of digital technology in transforming health and social care, underscoring both its potential and the barriers to its effective deployment. Despite the significant opportunities offered by digital solutions, their impact remains limited due to fragmented, small-scale interventions and a lack of strategic integration.
Key insights from the meeting emphasised the need for intentional investment, robust data utilisation, and overcoming cultural resistance within the workforce. Leaders stressed the importance of integrated approaches across digital, workforce, and prevention strategies, as well as the necessity of clear and coordinated financial planning.
The advent of AI, particularly generative AI, holds promise for enhancing service delivery and efficiency, but its success hinges on high-quality data and a well-prepared workforce. Ultimately, while technology is a powerful enabler, the human factor remains central. Effective transformation relies on changing mindsets and fostering relationships within the system. By aligning digital initiatives with strategic goals and maintaining a focus on human interaction, we can create a sustainable and effective health and social care system for the future.
Channel 3’s digital blueprint provides a comprehensive framework to address the issues raised by embedding digital tools within broader transformation strategies, focusing on patient journeys, and defining clear outcomes. But as mentioned previously, it’s a work in progress and we would like to engage practitioners and those with lived experience in developing it further. If the points raised in this article resonate with your own experience of digital transformation in health and care, and you would value exploring this in more detail, we’d love to hear from you.
Discover more digital health and social care perspectives


