
Meeting the healthcare needs of local populations through population health management is one of the core priorities for integrated care boards (ICBs). The strategic aims are to tailor better care and support for patients, design more sustainable health and care services and make better use of public resources.
In an effort to achieve these aims, many ICBs and their integrated care systems (ICSs) are now building the Index of Multiple Deprivation (IMD) into their geographical data.
IMD is based upon seven domain areas:
Income
Employment
Disability
Education
Crime
Housing
Local environment
Collectively these data sets determine where the poorest living standards are within a regional area and are cross-referenced against hospital patient data. Health professionals are then able to relate local areas of deprivation and whether there is a correlation to referral to treatment (RTT) pathways, associated waiting lists or clinical outcomes.
However, such analysis can only go so far as to help understand the cause and effects of local population health needs and their impact on local services. In fact, these shortcomings raise important questions, such as:
- How can health inequalities be aligned with local hospital planning to improve performance and social care needs?
- Which viable data sets can unlock local intelligence to inform all healthcare and social care providers to effectively redesign or prioritise their services?
- Healthcare and social care providers may be data-rich but struggle with digital maturity. How can improvements be embedded to make better use of the insights that data can offer?
Bridging the gap between data and delivery
To join the dots effectively between data and the delivery of a more focused service offering, the consideration of public health profiles is crucial. Only then can the full context of poor health outcomes, and the associated long-term conditions of the local populace, be understood.
Profiling health inequalities should inform how ICBs prioritise their commissioning intentions in future planning rounds.
To adapt pathways and service offerings to align with local needs, the first step is to look at what public health data are showing and consider the impact on the immediacy of hospital care. By joining the dots, you can begin to understand the causes of hospitalisation, and then work towards mitigating these causes. The aim is to reduce the number of patients ending up in a hospital within an emergency setting, on planned care pathways or on waiting lists, by pre-empting health service needs.
Taking a proactive approach to healthcare
By using local health profiles, which can be accessed via the Office for Health Improvement & Disparities website, health and social care professionals can align community and primary care services to the local prevalence of long-term conditions.
Here is an example of the insights that are provided:
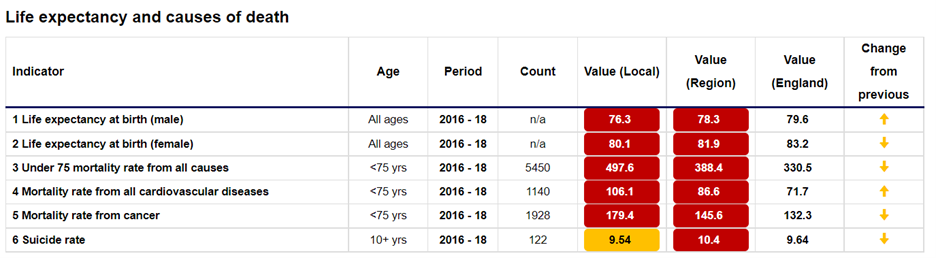
In this area, there is an identifiable need to focus on the health factors that affect cardiovascular diseases, cancer and suicide.
Local programmes and initiatives can be arranged at a community level to support people struggling with long-term conditions, such as:
- Proactive care planning
- Education
- Health screening
- Routine health checks.
By taking a proactive and data-first approach to healthcare, we can manage and control the cause and effects of these conditions. By doing so we empower the person to manage their condition, can stop it from getting worse, help them to understand the signals as to when early intervention is required and drastically reduce their chances of being admitted to hospital in an emergency.
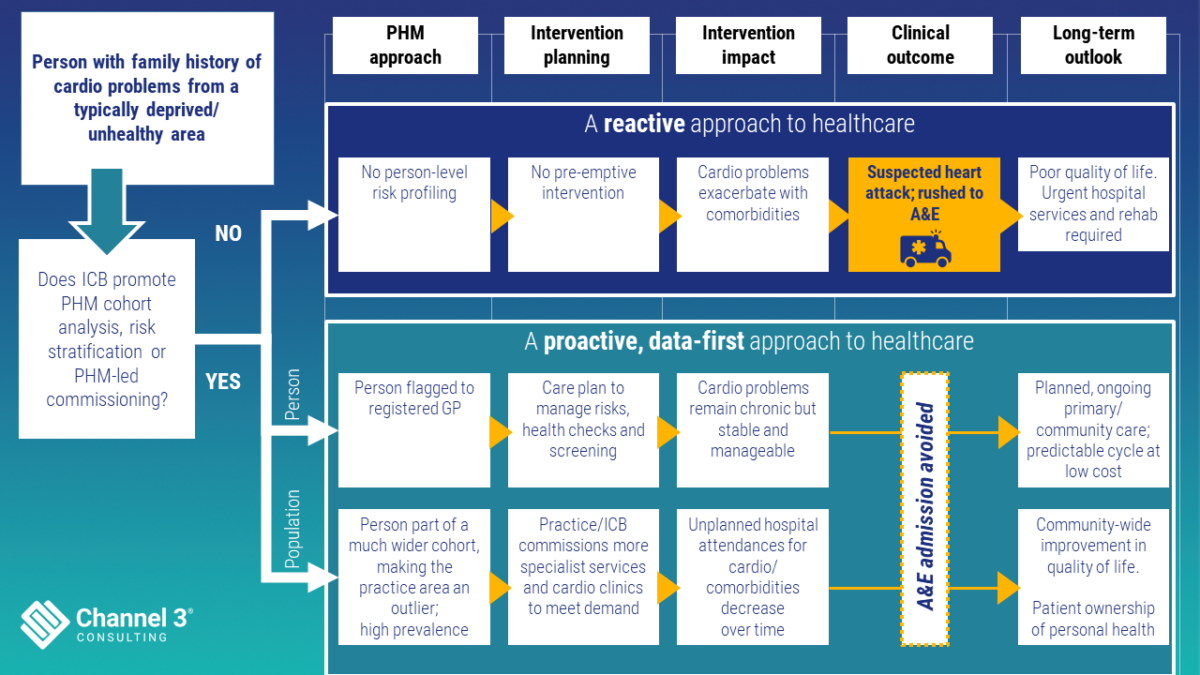
A population health management approach that reduces local health inequalities.
Once there is agreement on what needs to be monitored to improve the local population’s health, we can give clinicians the tools they need to monitor their local health inequalities gap and understand whether it is narrowing or widening.
At Channel 3 we found that it was possible to track the number of patients on the RTT waiting list and whether they would turn up at A&E with the same condition. Our approach covered one area of England:
- We found that there was a low percentage of RTT waiters who went on to visit A&E.
- From the data, we concluded that this low percentage was not due to a correlation with socio-economic factors or IMD category.
- Instead, of those patients who did present themselves at A&E, many of their conditions were related to hypertension, which is prevalent in the area in question.
It became clear that to reduce elective care activity, proactive care planning for hypertension needed earlier interventions, and it was important to treat associated disorders of hypertension at the earliest sign of detection.
Local health profiles have the power to provide the context needed to address the gaps in service provision, especially when driven by the CORE20Plus5 approach.
When health profiles and the right data are monitored, the results can be significant, unlocking improved health and well-being of local patients today as well as in years to come. Critically, at a time when waiting lists are causing logistical challenges, effective use of data can also reduce the burden on primary care and hospital services.
Channel 3 Consulting supports healthcare leaders to address the healthcare needs of their population. If you’re ready to discuss how you can harness the power of data to improve lives and deliver better care, please get in touch.
About the author – Mark O’Connor

Mark has operated across NHS healthcare in various executive positions, leading analytical teams for CSUs and has held positions such as Director of Commissioning Intelligence for NW London, Head of Information Services for Homerton Hospital, Head of Performance for United Lincolnshire Hospitals, Senior Technical Project Manager for the CQC and Public Health partner delivering dashboard reporting requirements for Covid19 responsiveness for Birmingham City Council. He has contributed to STP models of care and more recently the ICS commissioning planning round.
