Delivering on the Core20PLUS5 ambition requires an intricate understanding of the needs of the local population. Taking a data-first approach to population health management provides an opportunity to reduce health inequalities at both a national and system level. The COVID-19 pandemic shone a light on the extent of health inequalities in England. The sector must take decisive action or risk a further downturn in health outcomes, driving avoidable additional pressure on health services.
Tackling the inequality gap with Core20PLUS5
The Core20PLUS5 initiative is designed to drive targeted health inequalities and to help prioritise commissioning intentions for future integrated care planning:
Core 20
The most deprived 20% of the population in your region.
PLUS
Other population groups, identified by local population health data.
5
Targeting five clinical areas of health inequalities:
- Maternity: ensuring continuity of care for 75% of women from Black, Asian and minority ethnic communities and from the most deprived groups.
- Severe mental illness (SMI): ensuring annual health checks for 60% of those living with SMI.
- Chronic respiratory disease: a clear focus on Chronic Obstructive Pulmonary Disease (COPD) driving up the uptake of COVID, flu and pneumonia vaccines to reduce exacerbations and emergency hospital admissions due to those exacerbations.
- Early cancer diagnosis: 75% of cases diagnosed at stage 1 or 2 by 2028.
- Hypertension case-finding: to allow for interventions to optimise blood pressure and minimise the risk of myocardial infarction and stroke.
Core20PLUS5 infographic, NHS England:
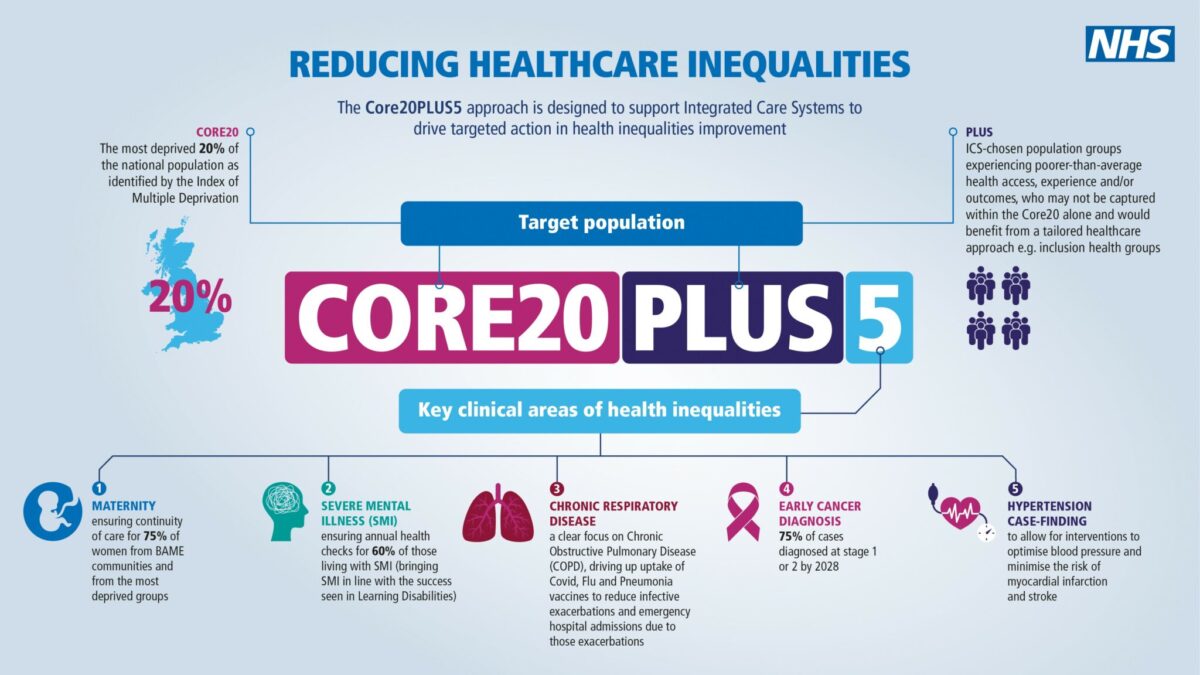
The Core20PLUS5 approach aims to contribute toward the overall government goal of increasing healthy life expectancy by five years by 2035 and is an excellent first step to creating lasting change that needs to be supported and applauded.
The power of data analysis to address health inequalities
The secret to the success of Core20Plus 5 lies in data. The numbers need to be analysed, and trends identified, to truly understand the population and build plans that meet their needs.
Whilst the public health agenda continues with joint strategic needs assessments, which locally profile population health outcomes, the connectivity between this work and commissioning alignment still has some way to go. Exploring this healthcare service data through careful analysis can help bridge the gap between what this data represents, at a system-wide and demographic level, and how this can be understood in the broader context of health inequalities.
The correlation of local health data and how to interpret it to improve population health outcomes is now widely accepted. In fact, there are now calls to strengthen opportunities for data analysts within the NHS by modernising their job and career development.
Professor Ben Goldacre MBE, Bennett Institute for Applied Data Science at the University of OxfordNHS data is a phenomenal resource that can revolutionise healthcare, research and the life sciences. But data alone is not enough. We need secure, efficient platforms – and teams with skills – to unleash this potential. This will be difficult, technical work. It is inspiring to see momentum grow for better, broader, safer use of health data across so many sectors
The COVID-19 pandemic showed us the value of local data and its capability to improve care services when collected and analysed accurately, before being submitted for national digestion. This momentum must be maintained and, if applied to the context of health inequalities, could provide a rich tapestry to help understand healthcare provision’s impact on local communities.
Now more than ever before, we can curate data that is timelier and more relevant. However, only through the analysis of this data can we truly understand the significance and power that is held in the data banks across our care systems. Simply put, when analysis guides service design, the results can be profound.
This approach is not novel. It is reminiscent of the pioneering studies undertaken by Dr John Snow, who in 1854 demonstrated the spread of disease back to its source. Using maps to plot his data, he tracked the spread of infections of Cholera outbreaks and proved to the world that the spread of infections was from a waterborne virus. In this case, the infections all stemmed from the distribution of infected drinking water provided by a water pump in Broad Street, London. The result of the logical interpretation of his analysis and survey-based data collections across London proved to the world the effectiveness of research and correlating data to establish the source of the spread of infections.
If a similar approach is applied, with modernised and advanced correlations, we too will better understand the nature of poor health, mainly attributed to areas of known deprivation, lifestyle behaviours and the impacts of the wider determinants of healthcare on our society.
Better lives. Better care. Better digital.
While Core20PLUS5 gives new impetus to reforming services across integrated care systems, it will not be a silver bullet for currently overwhelmed services. For real, lasting change, we must understand the correlation between the data and how it plays into the broader context of health inequalities. Without this insight, the risk of continual degradation of the health of local populations is real. Only through intelligent analysis will we reach the true potential to improve our health and the health of communities.
How does this move from practice to reality? How can health and care organisations deliver better health through data-driven healthcare and digital transformation?
At Channel 3, we have the relevant knowledge and first-hand experience to drive this change at a national and local level. We can work with you to align your data analysis requirements with your integrated care strategy and future commissioning intentions.
In practice, this approach could be used to understand patients’ conditions on a hospital’s waiting list to the nature and prevalence of conditions that are distinct to that hospital and their community. This is especially useful when considering the comorbidities that could have been managed better or prevented. Ultimately, there are a number of controllable factors that impact health. Lifestyle factors such as diet, fitness, smoking, living conditions and a person’s culture, all of which may affect their health. A data-first approach provides the necessary insights to take meaningful action against preventable conditions.
If you’re ready to discuss how you can harness the power of data to improve lives and deliver better care, please get in touch.
About the author

Mark O’Connor
Mark has operated across NHS healthcare in various executive positions, leading analytical teams for CSUs and has held positions such as Director of Commissioning Intelligence for NW London, Head of Information Services for Homerton Hospital, Head of Performance for United Lincolnshire Hospitals, Senior Technical Project Manager for the CQC and Public Health partner delivering dashboard reporting requirements for Covid19 responsiveness for Birmingham City Council.