We are approaching what is predicted to be “the toughest winter on record”. The combined prevalence of COVID-19, pneumonia and flu is contributing to an already pressurised situation in the NHS. Rising inflation, mortgages, fuel costs and other pressures are creating deep-seated socioeconomic problems which will inevitably result in pressures on our health and care system.
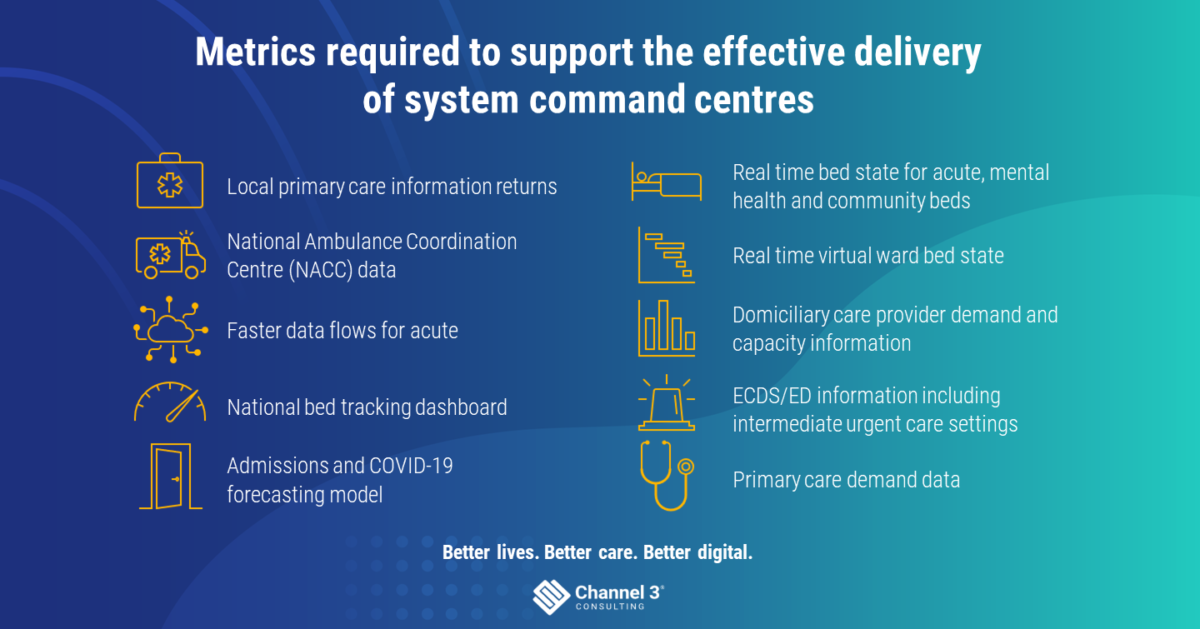
In preparation for this, NHS England is urging regions to set up data-driven “war rooms”. These new System Control Centres (SCCs) are expected to be created in every local area and operated on a 24/7 basis. Their purpose is to ensure visibility of, and a collective approach to, managing system demand and capacity across the country. Measures outlined in the SCC plan will enable the development of local hubs dedicated to serious respiratory infections, with patients receiving same-day access to care out of hospital, while also establishing additional capacity for hospitals and ambulance services. The guidance is prescriptive about the operating model and roles needed to operate the SCC and specifies potential data sources that should be available.
But the question is this:
Will a war room alone really help mitigate the risk of a bad winter, or should we also be focussing on getting data out onto the shop floor, where it can support real-time life-and-death decisions?
I would suggest there are three things that should be considered if you are trying to judge the success of an SCC:
1. Is there immediate visibility of a holistic patient record at the most pressured first points of care, such as in A&E, and is the data being used to change clinical and operational decision-making?
2. Is there a real-time, system-wide view of the patient across all local health and care stakeholders? Does that view enable clinicians, social workers and operational teams to understand of challenges, collaborate and take action? This is about more than the old-money daily Sitreps, using datasets that haven’t changed significantly in years and where the data is designed to track national targets. Instead, it’s about enabling clinical and operational staff to ask themselves things like “What’s the most important data I can share to enable my colleagues to take the best possible next decision about a person’s care?” and “How can I share that data most effectively?” Equally, with the reinvigorated desire for real-time data, we must all be aware of the risks of assuming real-time data is both clean and accurate enough to use as the basis for objective decisions.
3. Do your clinicians feel value in having data because you have designed the sharing of data and intelligence into the way they work and the systems they use? Having visibility of data across the care system is one thing, but to really drive change it needs to be actionable at the point of care. There is work to be done to make this so.
Success is attainable, but only if data lives in the pockets of clinicians and experts. I would argue this is at least as important – if not more so – than just having data in dashboards in a command centre.
What do I mean by that? Well, there are certain steps that need to be taken to ensure a systematic, consistent and collective approach to managing demand and capacity. As such, the building blocks of successful command centres would comprise the following elements:
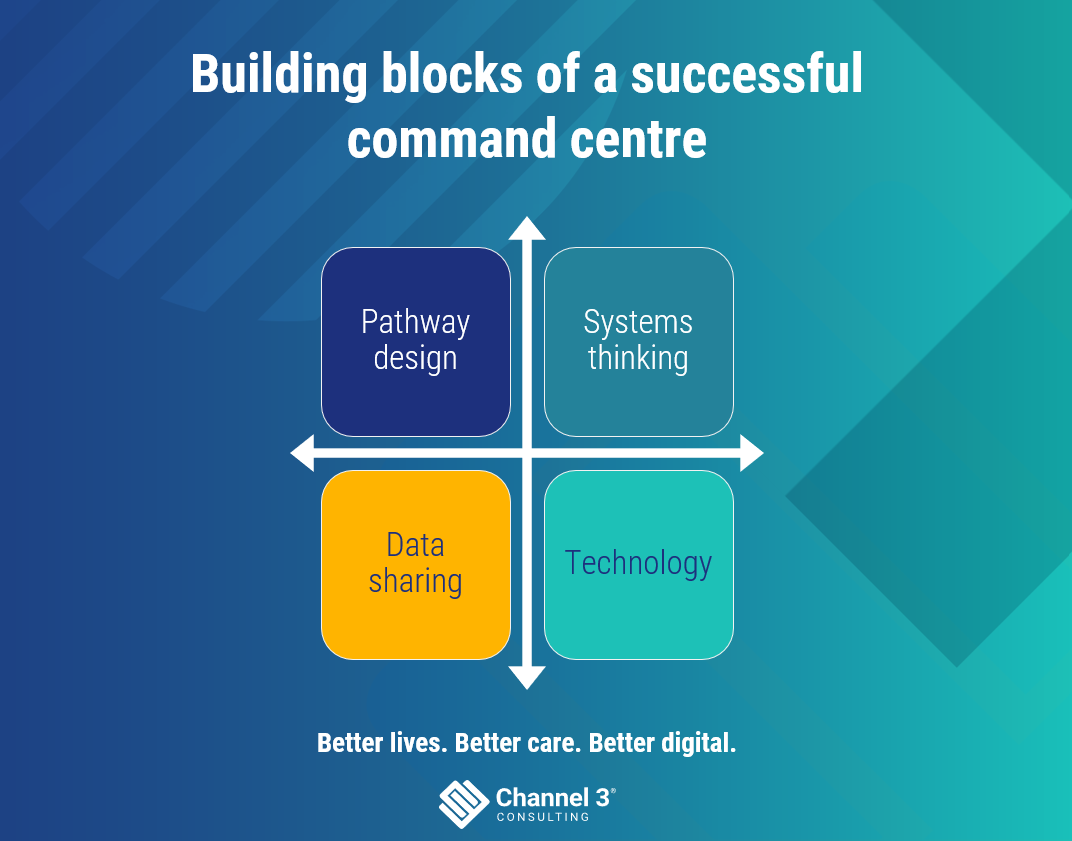
There are too many people trying to share too much data across too many different points of care and care teams, working in too diverse ways for a one-size-fits-all war room to enable effective working. Successful organisations are prioritising pathways and can see a golden thread of data from a regional view of activity to the data on the mobile device in the clinician’s pocket.
Further to this, some organisations have adopted a quality management system (QMS). They have taken a Lean approach to designing the way their organisation should work. As a result, they have defined a set of cascading indicators, which stem from the vision and values of their organisation. They have then embedded vital data systems that digitally enable care pathways, using the best tech for the job.
Having the right governance, technology and processes to enable data to flow freely from the point of origination to the points where it can be used.
Embedding data in clinical and operational workflow.
The regional System Control Centre timeline is a tight one
So, with only a month to go before the initiation of these control centres, here are three things that need to be done in the next two weeks:
1. Starting with the patient in mind and working backwards, pick priority care pathways and design data and tech-enabled blueprints to optimise care.
2. Catalogue your data assets so that you can identify where there are gaps in your ability to provide the right data that you need at the point of care.
3. Design your SCC in line with the operating model for winter, set up a war room and start populating screens with the data you have. However, also have a plan to replace outdated indicators and content with new data sets that you feel will really enable you to make the greatest impact at the point of care.
If you’re ready to discuss how you can harness the power of data to improve lives and deliver better care, please get in touch with us using the form below.
