There are not enough people to staff our health and social care system. Part of the problem lies in our workforce strategy, part of the problem lies in staff pay and working conditions, and another part arises from societal demands for support. Many agree that using technology more effectively can help to solve these people-related challenges, but what can technology do and how do you implement it without adding further pressure to your already stretched workforce?
Public sector staffing shortages hit health and social care from all angles
The staffing situation in the NHS and across the public sector is bleak. The care system needs to run like a clock, with many interdependent and fragile parts working together to address the societal issues of our time. Staff attrition is high, mental health issues and attempted suicide rates continue to escalate, and the popular press seems to be constantly attacking our GPs.
At the same time, demand for services is rising and even the investment available cannot always be spent because staff are burned out, we are still under the grip of COVID-19 and business as usual is crippling. While the spirit to transform exists, the flesh is weak due to a lack of capacity and capability in the right places.
Could patients be part of the health and care workforce?
An inability to maintain wellness within the general public creates additional patients on top of the existing high, and rising, demand. If patients can avoid the need for staffed NHS services, they effectively become part of the team. In this regard people and patients are a hidden health and care workforce. We need to encourage the public to ask themselves the question “Are we as well as we could be (given mind, body and societal constraints)?”
Whilst not everything is within their control, if patients and citizens were living their best lives, would that decrease demand on the NHS? Place of birth, standard of upbringing, mental and physical health are not always controllable factors. Clearly certain cogs in the clock are jammed by challenges in education, housing, employment, and the justice system as much as they are by lack of capacity in health and social care. That does not mean however that the pressure on the NHS cannot be alleviated to some extent through pre-emptive measures.
Pressure is testing the resolve of the most ardent staff
Some are arguing that the NHS simply needs more doctors and nurses. It is almost as if it would be easy to grow the capacity quickly and deploy them so they can bring down growing waiting lists. Yet a more sophisticated reading of the landscape is bound to point out that people who have wanted to be clinicians all their lives now feel under-valued, over-worked, asked to do things that they don’t want to do (or feel are necessary) and incumbered by poor technology.
Imagine having to farm in that landscape using only a few blunt hand tools when you see peers in other industries using the best machinery. Look more widely and the number of managers has fallen and there are fewer left to help, while sympathy for their predicament is at an all-time low. Staff who care more about their patients than themselves are asking whether they should remain in a career in the NHS?
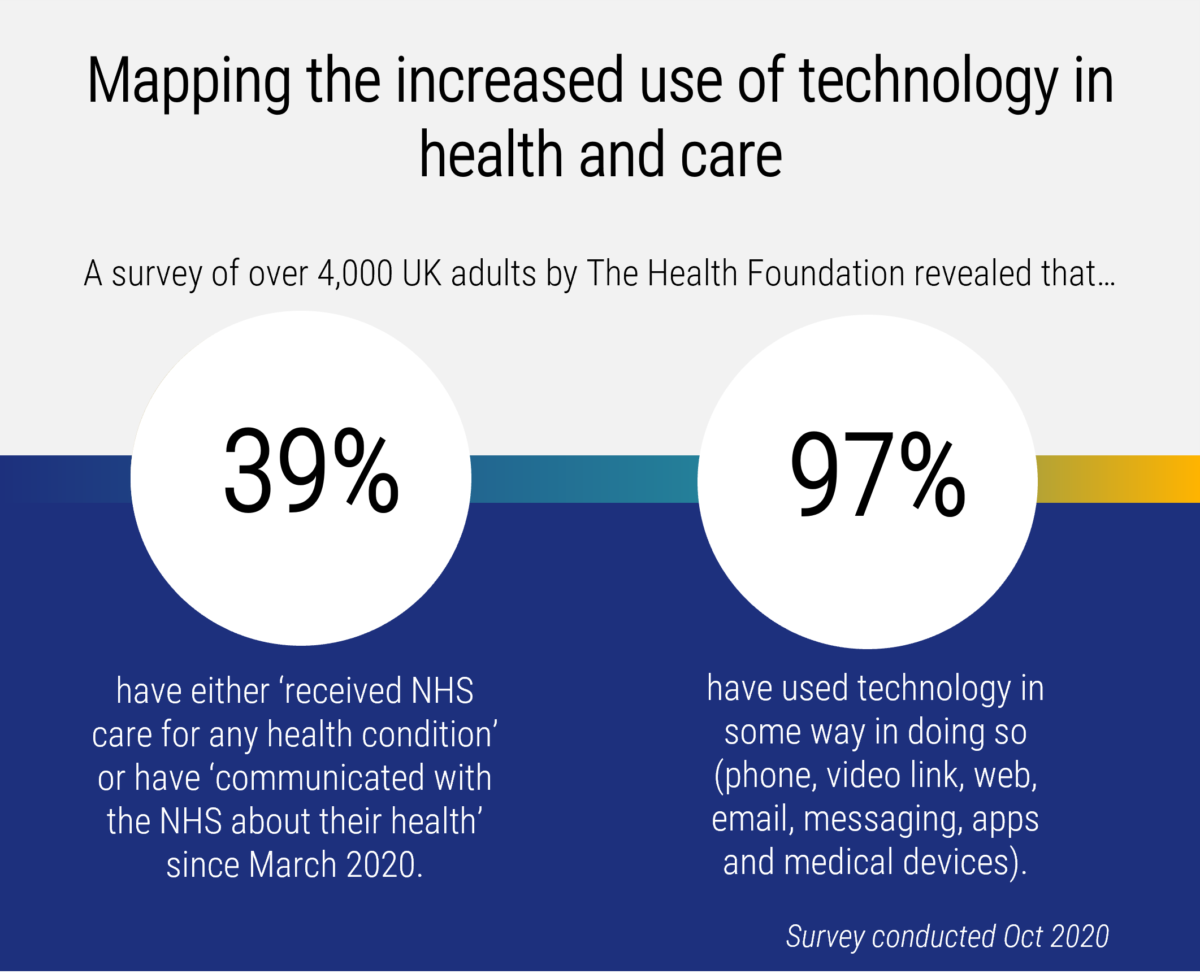
During the pandemic, part of the answer was to use technology
The national effort to fight COVID-19 was extraordinary for several reasons, not least the pace of the adoption of technology. Large amounts of new technology just worked. How did that happen? Determined groups of strategists, planners, commissioners, providers and some partners from industry were able to implement innovative tools that had been ready and waiting in the wings for some time.
The widespread adoption in primary care of new telephony, video consultation, online triage and other tooling was astonishing, and the momentum is being maintained. It wasn’t an accident that the technology worked. It was fuelled by new tools, often cloud-based, which made development faster.
The partnerships with industry leant more elbow-grease to the cause, with varying degrees of success. And the UK public sector quickly adopted the methods used by technology companies that quickly spot gaps in the market, create solutions that people want to use and get them to market .
Technology is not delivering its full potential to enrich working lives
In this context then, how do we sustain and grow the use of innovation to support staff wellbeing (by giving them the right tools to do their jobs), manage demand and automate some of the manual and paper processes that make life difficult? Further, how do we find the capacity to effect this change when day-to-day pressures are so acute?
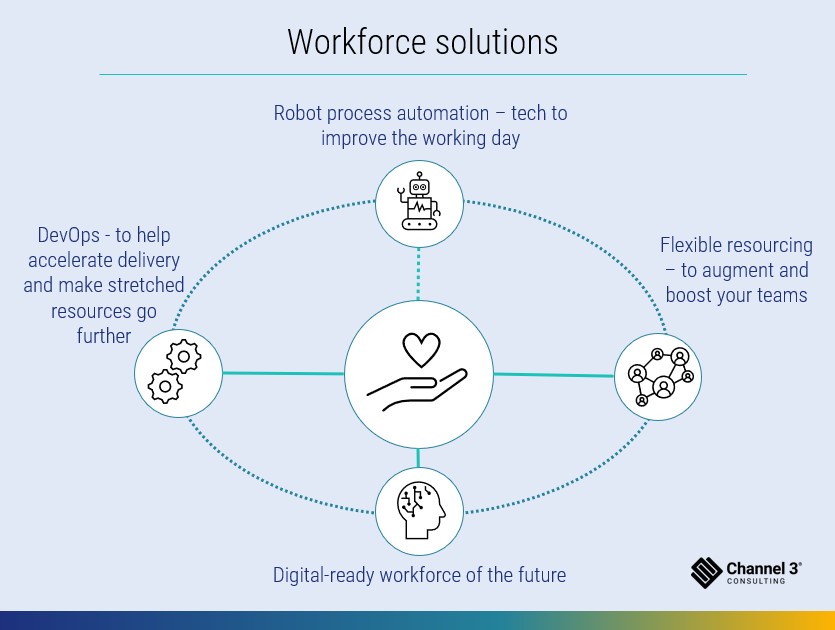
Channel 3 believes that some of the challenges faced can be addressed by thinking differently about:
The opportunity to use technology – especially the potential to use robotic process automation (RPA) to help staff be productive and potentially fill vacant roles.
Consider new models of resourcing to assist organisations that are trying innovative approaches.
Understand the potential for a DevOps approach to programme delivery (more of what that is later!).
Does a person need to do that job?
RPA, or using a computer to do routine and repetitive tasks, has landed well in many organisations’ back offices. A computer can check an invoice using basic rules and pass it for payment or reject it as effectively as a person can and without the risk of human error. This frees up staff resources for jobs that only a human can do, with the added benefits that the robots do not require annual leave and can work 24/7.
Equally, even with emerging artificial intelligence (AI), RPA is not yet ready to take nuanced and emotionally intelligent decisions – outside of laboratories – and so the deployment of RPA (the bots!) needs careful thought. For every article about AI adding emotional intelligence to RPA applications, there is a competing article expressing concern about the ethics and potential for bias in AI. There is still some way to go.
It can feel like the revolution is stuck in pilot-mode…
There have been great examples of new technology being piloted and delivering good early results but not being scaled or being transformational. The time it takes for technology to land in our sector – as opposed, for example, to the pace of adoption of Tik-Tok by the public – is reflective of the complexity of care settings and the diverse needs of our population. So, it is understandable to some extent. However, when considering the progress made by private sector organisations on robotic process automation then surely more can be done more quickly to mobilise a set of tools that can decrease the admin burden on clinicians.
…..but there are great examples of RPA in the NHS
We only need to look at the great work at the Royal Free Hospital to see the potential for RPA in the NHS. The team there has created a set of bots to do ever more sophisticated tasks that do not replace clinicians but do give clinical hours back to the organisation – this is how they measure productivity. It is brilliantly simple to discuss though quite difficult to do, and so if this piques your interest we would advise you to talk to them or contact us to learn more.
The robot is like the plough – it doesn’t replace the farmer
The most likely application of this kind of technology is to augment the role of physical staff, where it can improve the quality of a working day, decrease an admin burden and speed up processing. For example, early work has been done to improve the processing of referrals. In this case, RPA may prove as important an invention as the plough. It doesn’t replace the farmer (or the clinician in our environment), but it makes their job easier.
RPA is not a silver bullet and requires careful handling to land safely. Before embarking on an RPA project you need to be sure what you want from it, from people, process, technology, behaviour, culture and clinical outcomes perspectives. In our experience, vendor selection is also key, and you may need support from user experience consultancies like Channel 3 to make sure the technology can deliver on its promise and not further incumber your staff.
Sometimes you just need more farmers
Sometimes you just need more people to get transformation done. Hiring staff or even taking on fixed-term contractors, ostensibly with the skills and experience you need, can be an answer but it carries risk. The costs can be disproportionately high, the management burden can add to an already busy workload, the resources are often an unknown quantity and you need to keep them busy once you’ve committed to taking them on.
They also need to know your organisation and your third parties, have cultural alignment and be able to land and be productive from day one. The impact of sending an inexperienced member of staff to ask for a busy clinician’s time is huge in terms of the damage to internal relationships, project delivery, disruption to your core business and potential impact on patients.
Transformation staffing needs are highly seasonal and requirements change
Organisations like Channel 3 have found a new model for augmenting your team, where we run a bench of consultants that are managed, trained, vetted, and operate as part of our core team. So, when you ask for support, you can be sure that you are receiving somebody who is experienced and can be productive immediately. Like other organisations operating this flexible staffing model, we take on some of the risks of delivery and work as partners with you. The NHS may not need to employ more staff to support project work if this model is followed.
Organisations are adopting a DevOps approach to transformation
We see an increasing number of health and care organisations successfully use a “DevOps” approach to accelerate their transformation efforts – and make their stretched people resources go further. Amazon Web Services (AWS), a subsidiary of Amazon who provides on-demand cloud computing platforms and application programming interfaces (APIs), define DevOps as:
“The combination of cultural philosophies, practices, and tools that increases an organisation’s ability to deliver applications and services at high velocity: evolving and improving products at a faster pace than organisations using traditional software development and infrastructure management processes. This speed enables organisations to better serve their customers and compete more effectively in the market.”
The key to success with DevOps is to start with a ruthless focus of effort on delivering value to the person who will use the technology being developed and work back from there in continuous and fast review cycles to check that developments are staying true to our initial vision. Developers and operational staff are on the same team, working together and working more efficiently.
A DevOps approach can accelerate your programmes of work
Agile methodologies, which had their genesis in software development, are now impacting transformation programmes. Multi-disciplinary teams are getting on board with the idea of tearing down walls between the functions that own IT development and operations and the coalface of service delivery. This is improving how staff work with technology on a day-to-day basis so they can drive responsive and iterative unlocking of the value in technology.
Learning by doing, shortening cycle times, making improvements little and often are all techniques that are enabling organisations to be more digital and get more from their workforce. We at Channel 3 have seen that a DevOps approach is underpinning many of the achievements that were made so quickly, for example, during the darkest days of the pandemic.
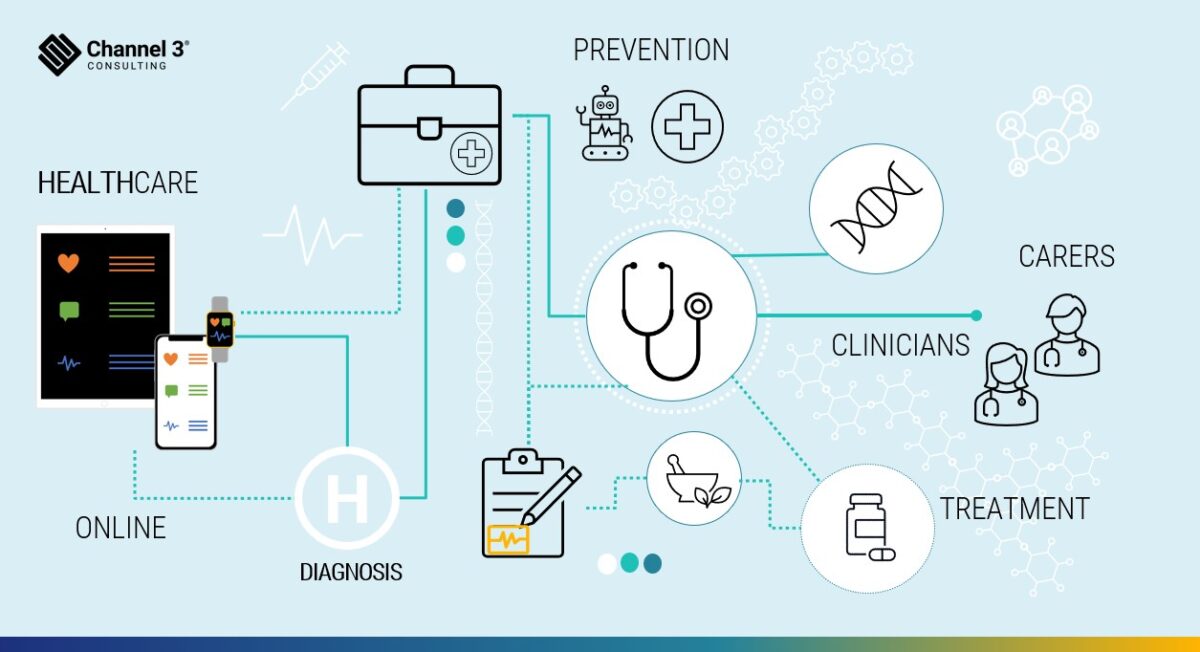
The health tech ecosystem
How do you manage people, ploughs and robots?
The impact of technology on organisational form, role definition, governance, process design and regulation have all been documented. Although we need illumination, much of the thinking has generated more heat than light. One thing is clear, the health and care sector needs a new operating model to take advantage of the opportunities that can be realised by creating a new digital workforce. It needs a workforce with digitally-savvy, well-supported staff where more tasks are automated so people don’t have to do them. We believe that health and care organisations should look beyond individual technology programmes to strategically plan, shape and reshape their workforces of the future to fully leverage the opportunities that a technology-enabled and intelligence driven health and care system has to offer.
If you’re tired of going to war, why not speak to us?
The arguments about the war for talent and the effectiveness of staffing models will rage on, and some health and social care staff will continue to be caught in the crossfire. This article is not addressing the issue of whether there are enough staff. Others have done the maths and walked the wards, and their arguments for more people are compelling.
However, we do feel that the sector could go some way to helping address the challenges through ramping up the use of technology, taking more flexible approaches to staffing projects and adopting a DevOps approach to moving transformation along at a faster pace. So, if you’re tired of going to war on talent in health and care, why not get in touch with us at Channel 3 to explore opportunities to do things differently?
